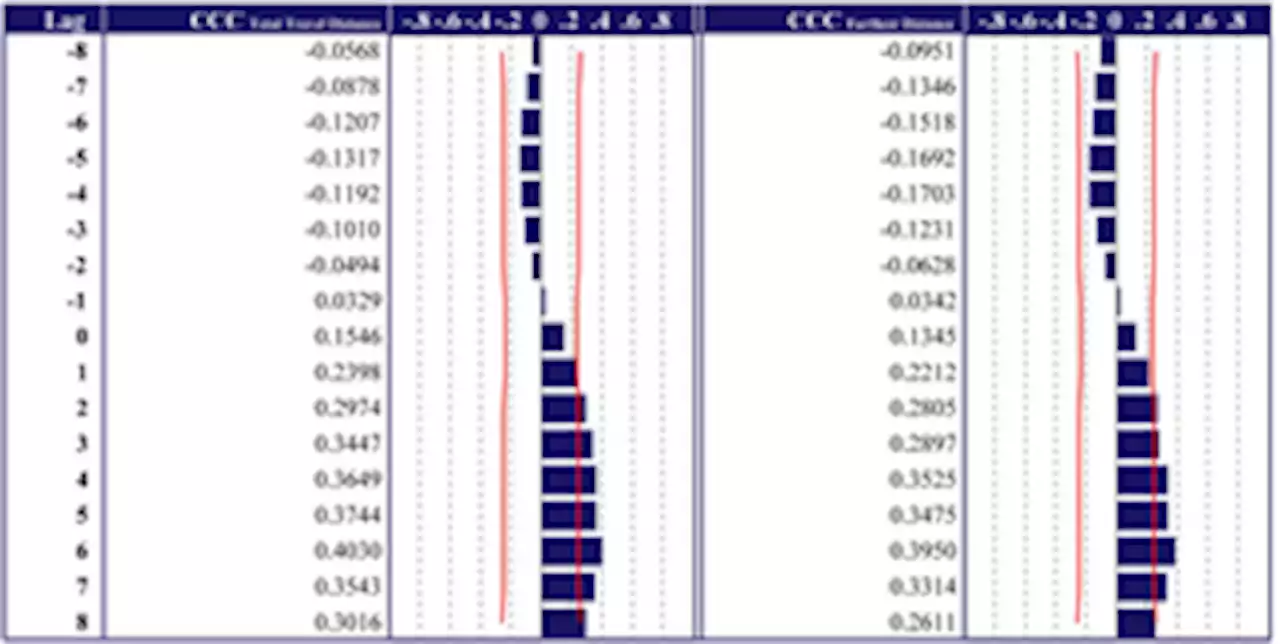
Is there a relationship between COVID-19 infections and everyday human mobility in metropolitan areas? PLOSONE
Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization,
Writing – original draft, Writing – review & editingDepartment of Housing and Environmental Design, Graduate School of Human Life and Ecology, Osaka Metropolitan University, Osaka, Japan
Belgique Dernières Nouvelles, Belgique Actualités
Similar News:Vous pouvez également lire des articles d'actualité similaires à celui-ci que nous avons collectés auprès d'autres sources d'information.
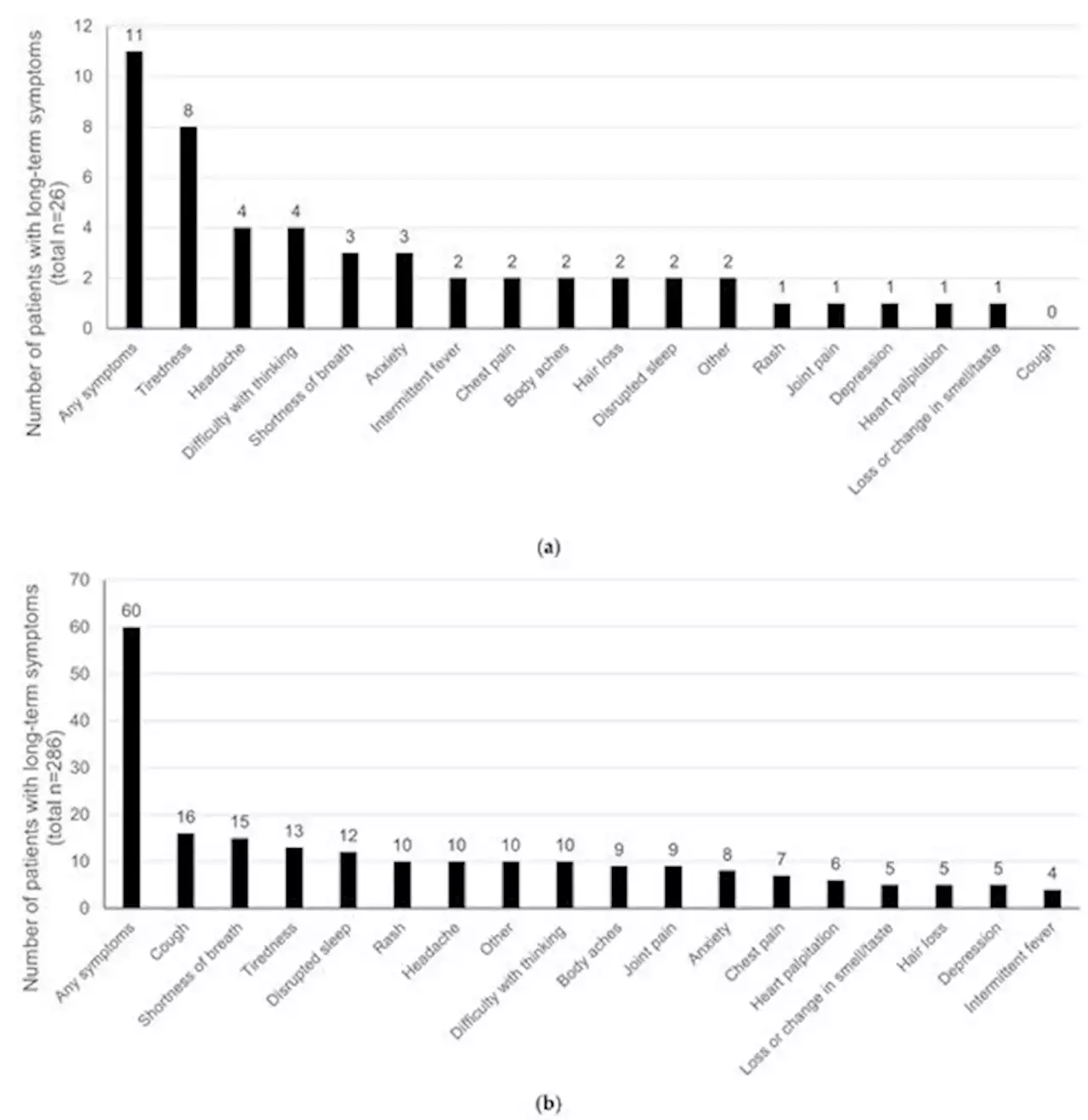 Comparison of Long-Term Complications of COVID-19 Illness among a Diverse Sample of Children by MIS-C StatusMost pediatric COVID-19 cases are asymptomatic; however, a small number of children are diagnosed with multisystem inflammatory syndrome in children (MIS-C), a rare but severe condition that is associated with SARS-CoV-2 infection. Persistent symptoms of COVID-19 illness in children diagnosed with/without MIS-C is largely unknown. A retrospective EHR review of patients with COVID-19 illness from one pediatric healthcare system to assess the presence of acute (<30 days) and chronic (≥30, 60–120, and >120 days) long-term COVID symptoms was conducted. Patients/caregivers completed a follow-up survey from March 2021 to January 2022 to assess the presence of long COVID. Results showed that non-MIS-C children (n=286; 54.49% Hispanic; 19.23% non-Hispanic Black; 5.77% other ethnicity; 79.49% government insurance) were younger (mean age 6.43 years [SD 5.95]) versus MIS-C (n=26) children (mean age 9.08 years, [SD 4.86]) (p=0.032). A share of 11.5% of children with MIS-C and 37.8% without MIS-C reported acute long COVID while 26.9% and 15.3% reported chronic long COVID, respectively. Females were almost twice as likely to report long symptoms versus males and those with private insurance were 66% less likely to report long symptoms versus those with government insurance. In conclusion, a substantial proportion of ethnically diverse children from low resource backgrounds with severe COVID illness are reporting long-term impacts. Findings can inform pediatric professionals about this vulnerable population in post-COVID-19 recovery efforts.
Comparison of Long-Term Complications of COVID-19 Illness among a Diverse Sample of Children by MIS-C StatusMost pediatric COVID-19 cases are asymptomatic; however, a small number of children are diagnosed with multisystem inflammatory syndrome in children (MIS-C), a rare but severe condition that is associated with SARS-CoV-2 infection. Persistent symptoms of COVID-19 illness in children diagnosed with/without MIS-C is largely unknown. A retrospective EHR review of patients with COVID-19 illness from one pediatric healthcare system to assess the presence of acute (<30 days) and chronic (≥30, 60–120, and >120 days) long-term COVID symptoms was conducted. Patients/caregivers completed a follow-up survey from March 2021 to January 2022 to assess the presence of long COVID. Results showed that non-MIS-C children (n=286; 54.49% Hispanic; 19.23% non-Hispanic Black; 5.77% other ethnicity; 79.49% government insurance) were younger (mean age 6.43 years [SD 5.95]) versus MIS-C (n=26) children (mean age 9.08 years, [SD 4.86]) (p=0.032). A share of 11.5% of children with MIS-C and 37.8% without MIS-C reported acute long COVID while 26.9% and 15.3% reported chronic long COVID, respectively. Females were almost twice as likely to report long symptoms versus males and those with private insurance were 66% less likely to report long symptoms versus those with government insurance. In conclusion, a substantial proportion of ethnically diverse children from low resource backgrounds with severe COVID illness are reporting long-term impacts. Findings can inform pediatric professionals about this vulnerable population in post-COVID-19 recovery efforts.
Lire la suite »
 Pathophysiology of Post-COVID syndromes: a new perspective - Virology JournalMost COVID-19 patients recovered with low mortality; however, some patients experienced long-term symptoms described as “long-COVID” or “Post-COVID syndrome” (PCS). Patients may have persisting symptoms for weeks after acute SARS-CoV-2 infection, including dyspnea, fatigue, myalgia, insomnia, cognitive and olfactory disorders. These symptoms may last for months in some patients. PCS may progress in association with the development of mast cell activation syndrome (MCAS), which is a distinct kind of mast cell activation disorder, characterized by hyper-activation of mast cells with inappropriate and excessive release of chemical mediators. COVID-19 survivors, mainly women, and patients with persistent severe fatigue for 10 weeks after recovery with a history of neuropsychiatric disorders are more prone to develop PCS. High D-dimer levels and blood urea nitrogen were observed to be risk factors associated with pulmonary dysfunction in COVID-19 survivors 3 months post-hospital discharge with the development of PCS. PCS has systemic manifestations that resolve with time with no further complications. However, the final outcomes of PCS are chiefly unknown. Persistence of inflammatory reactions, autoimmune mimicry, and reactivation of pathogens together with host microbiome alterations may contribute to the development of PCS. The deregulated release of inflammatory mediators in MCAS produces extraordinary symptoms in patients with PCS. The development of MCAS during the course of SARS-CoV-2 infection is correlated to COVID-19 severity and the development of PCS. Therefore, MCAS is treated by antihistamines, inhibition of synthesis of mediators, inhibition of mediator release, and inhibition of degranulation of mast cells.
Pathophysiology of Post-COVID syndromes: a new perspective - Virology JournalMost COVID-19 patients recovered with low mortality; however, some patients experienced long-term symptoms described as “long-COVID” or “Post-COVID syndrome” (PCS). Patients may have persisting symptoms for weeks after acute SARS-CoV-2 infection, including dyspnea, fatigue, myalgia, insomnia, cognitive and olfactory disorders. These symptoms may last for months in some patients. PCS may progress in association with the development of mast cell activation syndrome (MCAS), which is a distinct kind of mast cell activation disorder, characterized by hyper-activation of mast cells with inappropriate and excessive release of chemical mediators. COVID-19 survivors, mainly women, and patients with persistent severe fatigue for 10 weeks after recovery with a history of neuropsychiatric disorders are more prone to develop PCS. High D-dimer levels and blood urea nitrogen were observed to be risk factors associated with pulmonary dysfunction in COVID-19 survivors 3 months post-hospital discharge with the development of PCS. PCS has systemic manifestations that resolve with time with no further complications. However, the final outcomes of PCS are chiefly unknown. Persistence of inflammatory reactions, autoimmune mimicry, and reactivation of pathogens together with host microbiome alterations may contribute to the development of PCS. The deregulated release of inflammatory mediators in MCAS produces extraordinary symptoms in patients with PCS. The development of MCAS during the course of SARS-CoV-2 infection is correlated to COVID-19 severity and the development of PCS. Therefore, MCAS is treated by antihistamines, inhibition of synthesis of mediators, inhibition of mediator release, and inhibition of degranulation of mast cells.
Lire la suite »
 Risk of thyroid dysfunction associated with mRNA and inactivated COVID-19 vaccines: a population-based study of 2.3 million vaccine recipients - BMC MedicineBackground In view of accumulating case reports of thyroid dysfunction following COVID-19 vaccination, we evaluated the risks of incident thyroid dysfunction following inactivated (CoronaVac) and mRNA (BNT162b2) COVID-19 vaccines using a population-based dataset. Methods We identified people who received COVID-19 vaccination between 23 February and 30 September 2021 from a population-based electronic health database in Hong Kong, linked to vaccination records. Thyroid dysfunction encompassed anti-thyroid drug (ATD)/levothyroxine (LT4) initiation, biochemical picture of hyperthyroidism/hypothyroidism, incident Graves’ disease (GD), and thyroiditis. A self-controlled case series design was used to estimate the incidence rate ratio (IRR) of thyroid dysfunction in a 56-day post-vaccination period compared to the baseline period (non-exposure period) using conditional Poisson regression. Results A total of 2,288,239 people received at least one dose of COVID-19 vaccination (57.8% BNT162b2 recipients and 42.2% CoronaVac recipients). 94.3% of BNT162b2 recipients and 92.2% of CoronaVac recipients received the second dose. Following the first dose of COVID-19 vaccination, there was no increase in the risks of ATD initiation (BNT162b2: IRR 0.864, 95% CI 0.670–1.114; CoronaVac: IRR 0.707, 95% CI 0.549–0.912), LT4 initiation (BNT162b2: IRR 0.911, 95% CI 0.716–1.159; CoronaVac: IRR 0.778, 95% CI 0.618–0.981), biochemical picture of hyperthyroidism (BNT162b2: IRR 0.872, 95% CI 0.744–1.023; CoronaVac: IRR 0.830, 95% CI 0.713–0.967) or hypothyroidism (BNT162b2: IRR 1.002, 95% CI 0.838–1.199; CoronaVac: IRR 0.963, 95% CI 0.807–1.149), GD, and thyroiditis. Similarly, following the second dose of COVID-19 vaccination, there was no increase in the risks of ATD initiation (BNT162b2: IRR 0.972, 95% CI 0.770–1.227; CoronaVac: IRR 0.879, 95%CI 0.693–1.116), LT4 initiation (BNT162b2: IRR 1.019, 95% CI 0.833–1.246; CoronaVac: IRR 0.768, 95% CI 0.613–0.962), hyperthyroidism (BNT162b2: IRR 1.0
Risk of thyroid dysfunction associated with mRNA and inactivated COVID-19 vaccines: a population-based study of 2.3 million vaccine recipients - BMC MedicineBackground In view of accumulating case reports of thyroid dysfunction following COVID-19 vaccination, we evaluated the risks of incident thyroid dysfunction following inactivated (CoronaVac) and mRNA (BNT162b2) COVID-19 vaccines using a population-based dataset. Methods We identified people who received COVID-19 vaccination between 23 February and 30 September 2021 from a population-based electronic health database in Hong Kong, linked to vaccination records. Thyroid dysfunction encompassed anti-thyroid drug (ATD)/levothyroxine (LT4) initiation, biochemical picture of hyperthyroidism/hypothyroidism, incident Graves’ disease (GD), and thyroiditis. A self-controlled case series design was used to estimate the incidence rate ratio (IRR) of thyroid dysfunction in a 56-day post-vaccination period compared to the baseline period (non-exposure period) using conditional Poisson regression. Results A total of 2,288,239 people received at least one dose of COVID-19 vaccination (57.8% BNT162b2 recipients and 42.2% CoronaVac recipients). 94.3% of BNT162b2 recipients and 92.2% of CoronaVac recipients received the second dose. Following the first dose of COVID-19 vaccination, there was no increase in the risks of ATD initiation (BNT162b2: IRR 0.864, 95% CI 0.670–1.114; CoronaVac: IRR 0.707, 95% CI 0.549–0.912), LT4 initiation (BNT162b2: IRR 0.911, 95% CI 0.716–1.159; CoronaVac: IRR 0.778, 95% CI 0.618–0.981), biochemical picture of hyperthyroidism (BNT162b2: IRR 0.872, 95% CI 0.744–1.023; CoronaVac: IRR 0.830, 95% CI 0.713–0.967) or hypothyroidism (BNT162b2: IRR 1.002, 95% CI 0.838–1.199; CoronaVac: IRR 0.963, 95% CI 0.807–1.149), GD, and thyroiditis. Similarly, following the second dose of COVID-19 vaccination, there was no increase in the risks of ATD initiation (BNT162b2: IRR 0.972, 95% CI 0.770–1.227; CoronaVac: IRR 0.879, 95%CI 0.693–1.116), LT4 initiation (BNT162b2: IRR 1.019, 95% CI 0.833–1.246; CoronaVac: IRR 0.768, 95% CI 0.613–0.962), hyperthyroidism (BNT162b2: IRR 1.0
Lire la suite »
 Can adherence to COVID-19 mitigation measures be predicted using cognitive variables?In a new study, researchers investigated the correlations between cognitive variables such as self-control, impulsivity, and future orientation and disease mitigation behaviors associated with the coronavirus disease 2019 (COVID-19) pandemic.
Can adherence to COVID-19 mitigation measures be predicted using cognitive variables?In a new study, researchers investigated the correlations between cognitive variables such as self-control, impulsivity, and future orientation and disease mitigation behaviors associated with the coronavirus disease 2019 (COVID-19) pandemic.
Lire la suite »
 WWE boss Triple H tests positive for Covid-19 and will miss tonight's RawBREAKING: WWE boss Triple H has reportedly tested positive for Covid-19 and will miss tonight’s episode of Raw.
WWE boss Triple H tests positive for Covid-19 and will miss tonight's RawBREAKING: WWE boss Triple H has reportedly tested positive for Covid-19 and will miss tonight’s episode of Raw.
Lire la suite »